Angioplasty and stent - heart - discharge
Drug-eluting stents - discharge; PCI - discharge; Percutaneous coronary intervention - discharge; Balloon angioplasty - discharge; Coronary angioplasty - discharge; Coronary artery angioplasty - discharge; Cardiac angioplasty - discharge; PTCA - discharge; Percutaneous transluminal coronary angioplasty - discharge; Heart artery dilatation - discharge; Angina angioplasty - discharge; Heart attack angioplasty - discharge; CAD angioplasty - dischargeDrug-eluting stents - discharge; PCI - discharge; Percutaneous coronary intervention - discharge; Balloon angioplasty - discharge; Coronary angioplasty - discharge; Coronary artery angioplasty - discharge; Cardiac angioplasty - discharge; PTCA - discharge; Percutaneous transluminal coronary angioplasty - discharge; Heart artery dilatation -...
The Basics
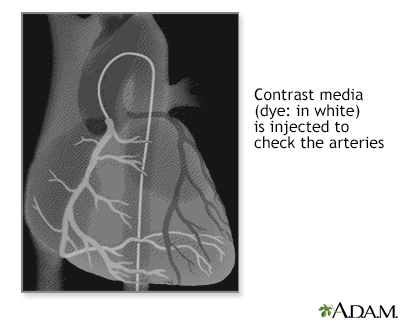
Tests for coronary artery blockage
A Closer Look
Directional coronary atherectomy (DCA) - Animation
Directional coronary atherectomy (DCA)
Animation
Percutaneous transluminal coronary angioplasty (PTCA) - Animation
Percutaneous transluminal coronary angioplasty (PTCA)
Animation
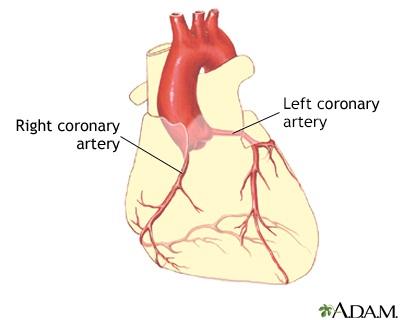
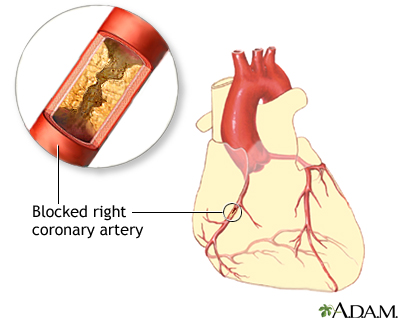
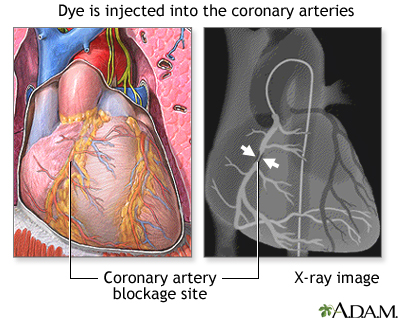
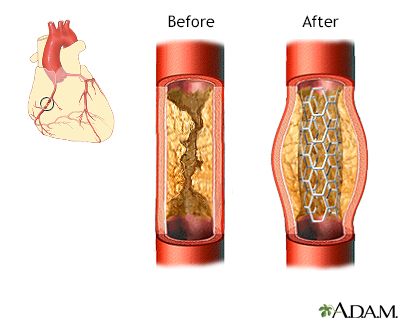
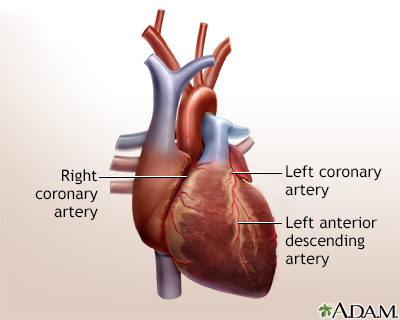
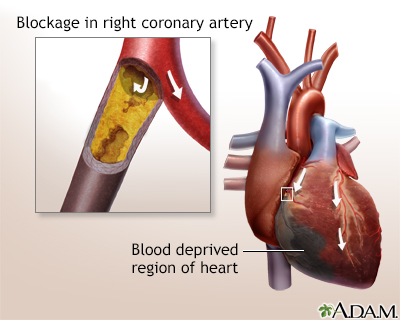
Coronary artery blockage
Atherosclerosis is a common disorder of the arteries. Fat, cholesterol, and other substances collect in the walls of arteries. Larger accumulations are called atheromas or plaque and can damage artery walls and block blood flow. Severely restricted blood flow in the heart muscle leads to symptoms such as chest pain.
Coronary artery blockage
illustration
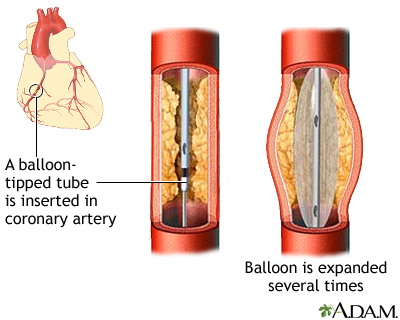
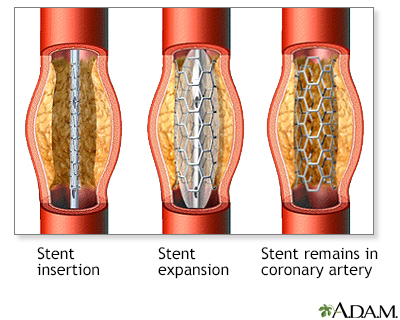
Coronary artery balloon angioplasty - series
Presentation
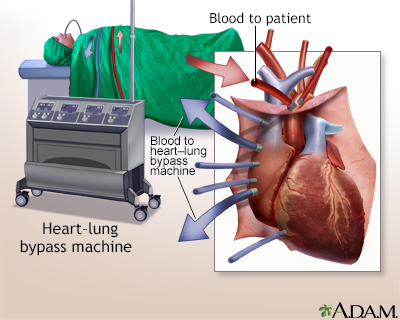
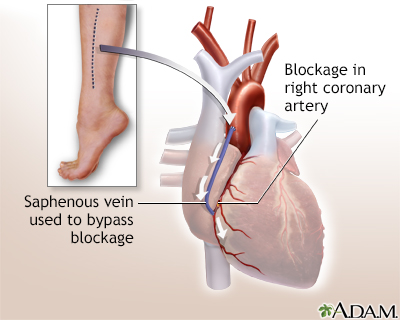
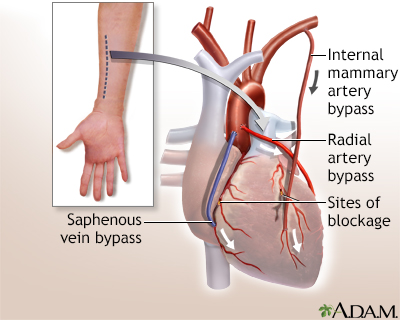
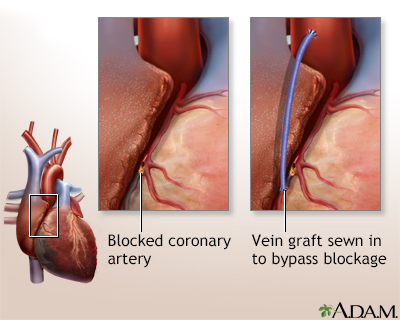
Heart bypass surgery - series
Presentation
Directional coronary atherectomy (DCA) - Animation
Directional coronary atherectomy (DCA)
Animation
Percutaneous transluminal coronary angioplasty (PTCA) - Animation
Percutaneous transluminal coronary angioplasty (PTCA)
Animation
Coronary artery blockage
Atherosclerosis is a common disorder of the arteries. Fat, cholesterol, and other substances collect in the walls of arteries. Larger accumulations are called atheromas or plaque and can damage artery walls and block blood flow. Severely restricted blood flow in the heart muscle leads to symptoms such as chest pain.
Coronary artery blockage
illustration
Coronary artery balloon angioplasty - series
Presentation
Heart bypass surgery - series
Presentation
Angioplasty and stent - heart - discharge
Drug-eluting stents - discharge; PCI - discharge; Percutaneous coronary intervention - discharge; Balloon angioplasty - discharge; Coronary angioplasty - discharge; Coronary artery angioplasty - discharge; Cardiac angioplasty - discharge; PTCA - discharge; Percutaneous transluminal coronary angioplasty - discharge; Heart artery dilatation - discharge; Angina angioplasty - discharge; Heart attack angioplasty - discharge; CAD angioplasty - dischargeDrug-eluting stents - discharge; PCI - discharge; Percutaneous coronary intervention - discharge; Balloon angioplasty - discharge; Coronary angioplasty - discharge; Coronary artery angioplasty - discharge; Cardiac angioplasty - discharge; PTCA - discharge; Percutaneous transluminal coronary angioplasty - discharge; Heart artery dilatation -...
The Basics
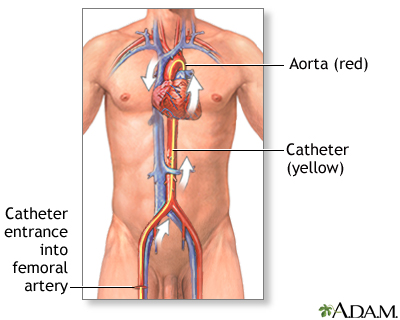
Tests for coronary artery blockage
A Closer Look
Angioplasty and stent - heart - discharge
Drug-eluting stents - discharge; PCI - discharge; Percutaneous coronary intervention - discharge; Balloon angioplasty - discharge; Coronary angioplasty - discharge; Coronary artery angioplasty - discharge; Cardiac angioplasty - discharge; PTCA - discharge; Percutaneous transluminal coronary angioplasty - discharge; Heart artery dilatation - discharge; Angina angioplasty - discharge; Heart attack angioplasty - discharge; CAD angioplasty - dischargeDrug-eluting stents - discharge; PCI - discharge; Percutaneous coronary intervention - discharge; Balloon angioplasty - discharge; Coronary angioplasty - discharge; Coronary artery angioplasty - discharge; Cardiac angioplasty - discharge; PTCA - discharge; Percutaneous transluminal coronary angioplasty - discharge; Heart artery dilatation -...
The Basics
Tests for coronary artery blockage
A Closer Look
Review Date: 8/16/2022
Reviewed By: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.